The term “Neoantigens” refers to antigens that have not been previously recognized by the immune system. Hence, they are newly formed antigens.
Over time, cancer and tumor cells accumulate mutations leading to the production of mutated proteins. Genome sequencing revealed that newly initiated cancer cells acquire tens to thousands of different somatic mutations. The number of mutations increases as cancer progresses. Most of the mutations give cancer an advantage to grow and often results in genomic instability. As of 2017, approximately 140 genes have been identified that are involved in tumorigenesis. Tumorigenesis is the gradual loss of original cell identity. During tumorigenesis, normal cells gain properties that can make these cells malignant.
Somatic mutations can alter amino acid coding sequences (nonsynonymous mutations), resulting in the expression of mutant proteins in tumors. The abnormal proteins are processed into short peptides called epitopes. The cell's machinery presents these peptides on the cell surface via the major histocompatibility complex (MHC). The MHC offers the epitopes as foreign antigens (neoantigens) to T cells. MHC is also knowns as human leukocyte antigen (HLA) in humans.
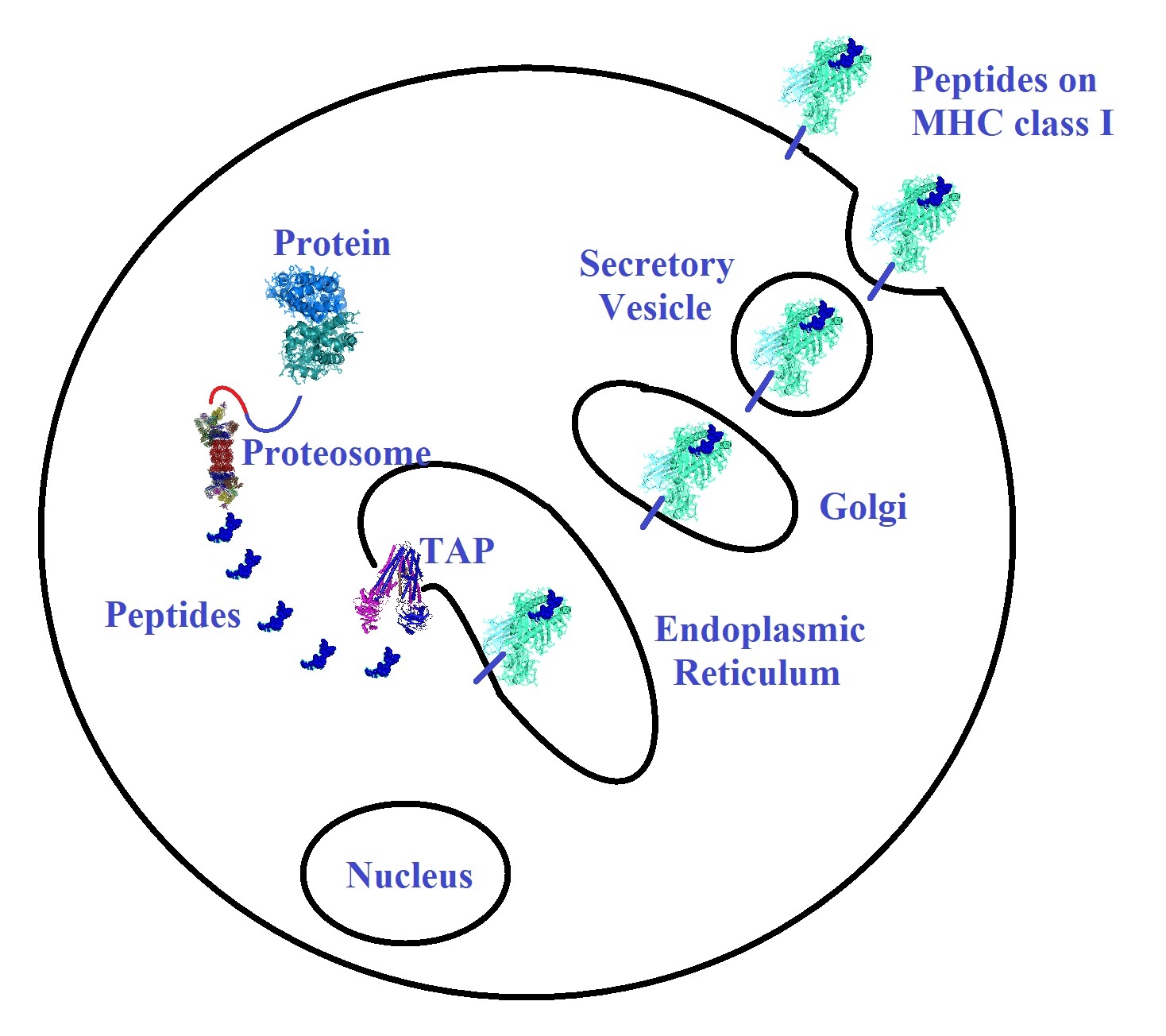
Figure 1: Tumor antigen processing and presentation on MHC class I
To kill established cancer cells, CD8+ T effector cells need to recognize antigens displayed by major histocompatibility complex (MHC) class I molecules on tumor cells. Endogenously synthesized proteins are tagged or ubiquitylated and degraded by the proteasome into short peptides of 8 to 11 amino acids in length. Peptides enter the endoplasmic reticulum (ER) by way of the transporter associated with antigen processing (TAP) complex. In the ER, peptides bind with variable affinities to MHC class I. The MHC class I peptide complexes are delivered to the plasma membrane through the Golgi complex. CD8+ cytotoxic T cells can recognize peptides presented at the plasma membrane. Some T cells recognize peptides shared between normal and tumor cells. However, T cell receptors tend to bind with a higher affinity to neoantigens. Tumors expressing higher numbers of neoantigens are more likely to induce immune-mediated tumor elimination. The MHC class II system works in a similar way, but longer peptides with 11 to 22 amino acids or longer are presented on antigen-presenting cells
Reference
Cao, Y. Tumorigenesis as a process of gradual loss of original cell identity and gain of properties of neural precursor/progenitor cells. Cell Biosci 7, 61 (2017). [BMC]
Smith KJ, Pyrdol J, Gauthier L, Wiley DC, Wucherpfennig KW. Crystal structure of HLA-DR2 (DRA*0101, DRB1*1501) complexed with a peptide from human myelin basic protein. J Exp Med. 1998 Oct 19;188(8):1511-20. [PMC]
T cell defined human tumor antigens
Yarchoan M, Johnson BA 3rd, Lutz ER, Laheru DA, Jaffee EM. Targeting neoantigens to augment antitumour immunity. Nat Rev Cancer. 2017 Apr;17(4):209-222. [Nature Reviews Cancer]
Yuan J, Hegde PS, Clynes R, Foukas PG, Harari A, Kleen TO, Kvistborg P, Maccalli C, Maecker HT, Page DB, Robins H, Song W, Stack EC, Wang E, Whiteside TL, Zhao Y, Zwierzina H, Butterfield LH, Fox BA. Novel technologies and emerging biomarkers for personalized cancer immunotherapy. J Immunother Cancer. 2016 Jan 19;4:3. [PMC]
---...---